THE RISK MANAGEMENT OF THE PHARMACY PREPARATIONS IN THE HOSPITAL PHARMACIES (submitted in 2019)
Pdf

European Statement
Production and Compounding
Author(s)
ADRIANA DURCANSKA
Why was it done?
The quality and safety standards of pharmacy preparations are not harmonised throughout Europe. They fall under the national competencies of individual European countries.
What was done?
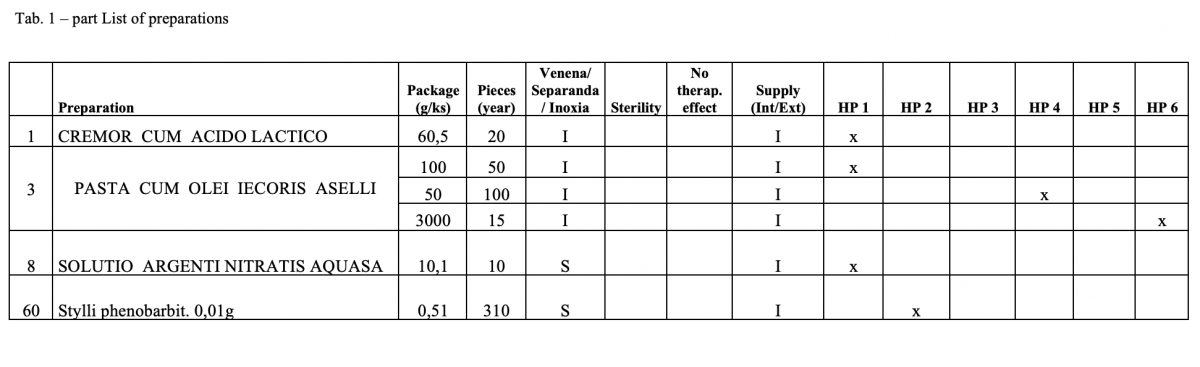
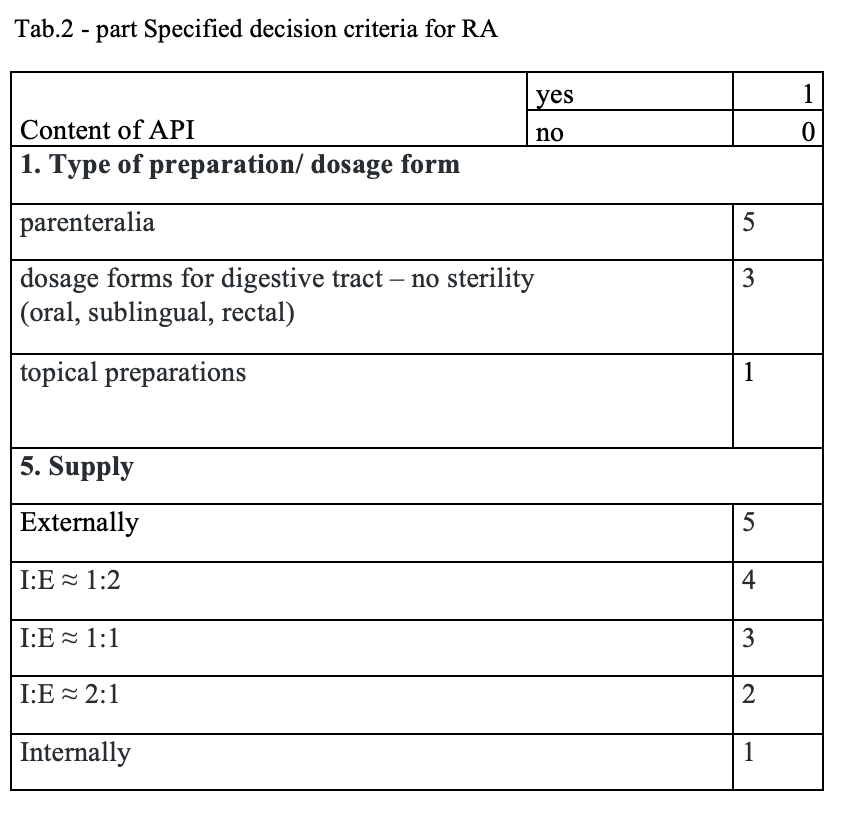
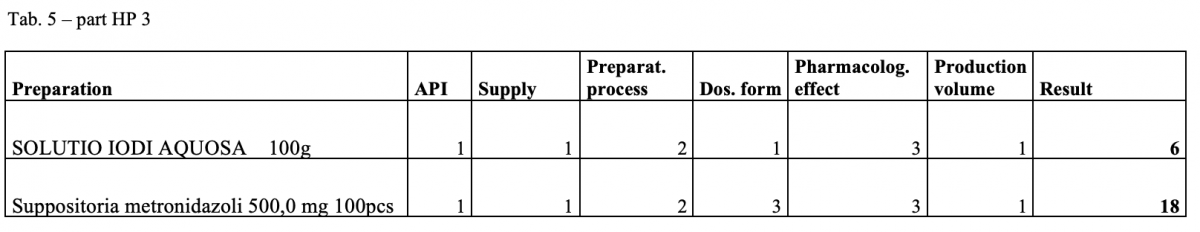
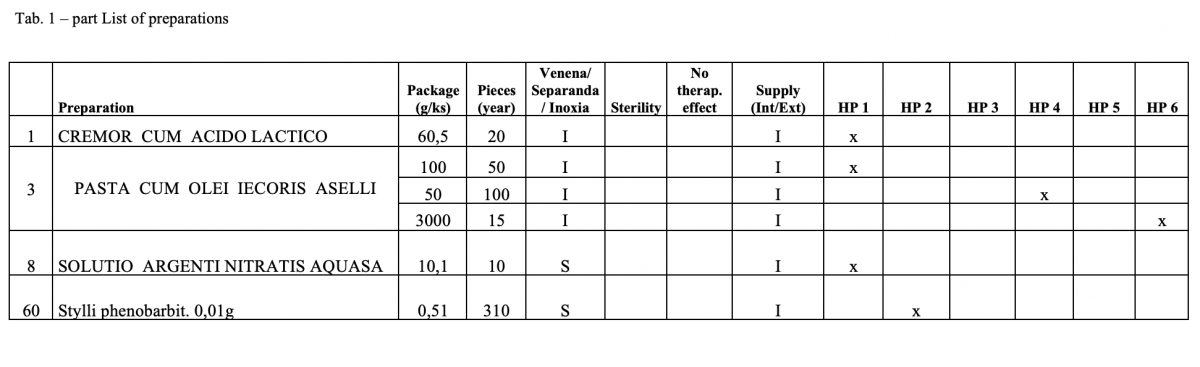
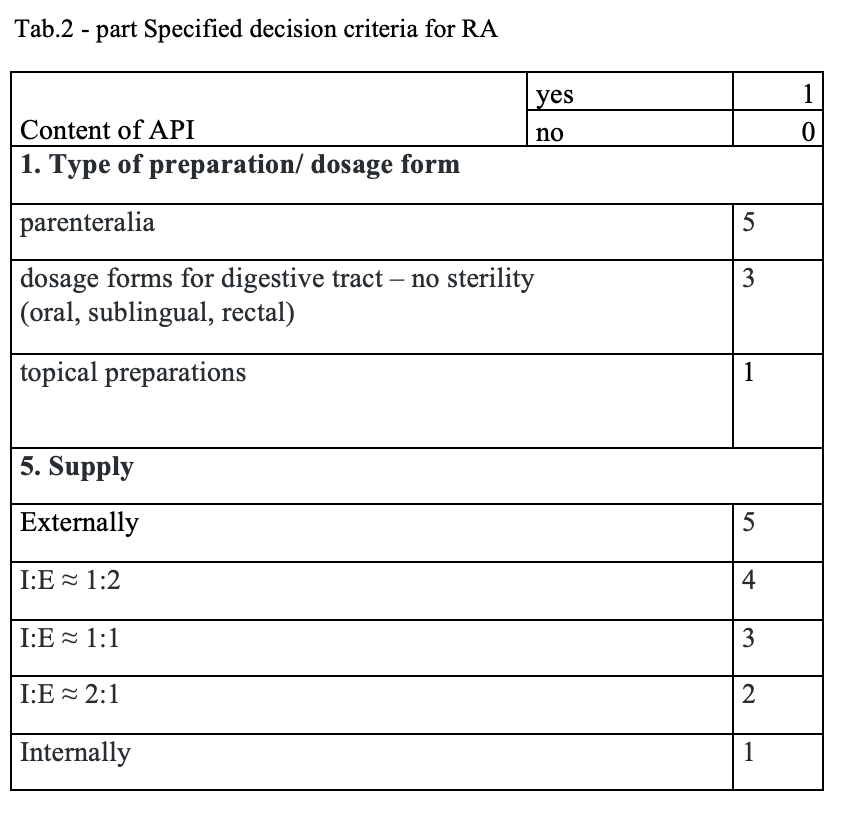
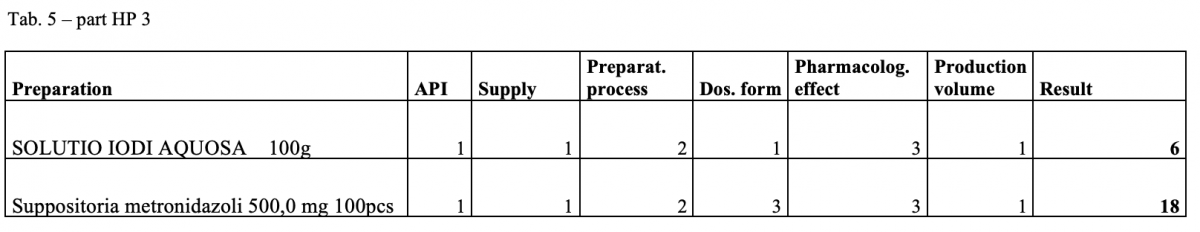
The quantitative risk assessment of the pharmacy preparations for stock in hospital pharmacies (HPs) in accordance with Resolution EDQM CM / Res (2016) 1; to specify the decision criteria for the risk assessment; the risk management of the pharmacy preparations for stock in the country; to design a check list of the risk assessment for extempore preparations.
How was it done?
Out of the total number of 53 hospital pharmacies contacted, 5 pharmacies sent a suitable file.
What has been achieved?
A total of 170 types of medicines are being prepared in HPs. One HP had the result of the risk ≥ 100 when preparing ophthalmic medicines. Annex A is a check list designed to assess the risk of extempore preparations.
What next?
The management is and will be forced to consider its introduction or to use another model: hospital – GMP / outsourcing / central pharmacy preparing and distributing. The aim of using the document in hospital pharmacies of the country.
TEMPERATURE AND RELATIVE HUMIDITY CONTROL IN THE PACKAGING ENCLOSURE OF SOLID ORAL DOSAGE FORMS (submitted in 2019)
Pdf

European Statement
Production and Compounding
Author(s)
María Lourdes Recio Blázquez, José Manuel Martínez Sesmero, Lidia Ybáñez García, Gonzalo Hernando Llorente, María Molinero Muñoz
Why was it done?
The purpose is to control two environmental conditions to guarantee the comfort of the workforce and the quality of the finished product quality. 519,321 SODFs have been repackaged in unit doses last year. The 8% of the SODFs come from multidose containers that have been exposed to environmental temperature and humidity during this process. Employees have been exposed to identical conditions.
What was done?
A temperature (t) and relative humidity (RH) control system has been established in the enclosure where the solid oral dosage forms (SODFs) are packaged in unit doses.
How was it done?
Among the diversity of hygrometric sensors commercialised, a device equipped with a condenser was chosen. The operation is based on modifying the capacity when varying the dielectric constant of the medium, in this case, due to varying the amount of water contained in the air between the plates. – C = ε A / D – C: capacity value. – ε: dielectric constant. – A: area of the condenser plates. – D: distance between the condenser plates. The device also incorporates a temperature sensor. The t (ºC) and RH of each moment are shown, for visual inspection, on the device screen. The data obtained with certain time frequency can be stored on a Secure Digital memory card and be downloaded on a computer that has that program installed (on spreadsheet format) helping to obtain graphics as well.
What has been achieved?
The range of t (ºC) has remained stable between 26 and 24ºC for 6 months, with minimal variations from maximum 28.5ºC to minimum 23.4ºC. The UNE 100713: 2005 is met. RH has been below 45% during 68% of the days worked, which has favored the repackaging of the units affected by humidity but not the worker. The range of RH has varied between 56.3% and 23.6%, not complying with the UNE 100713: 2005 standard.
What next?
Metabolic rate, clothing insulation, air temperature, radiant temperature, air speed and humidity shall be addressed when defining conditions for acceptable thermal comfort. It would be helpful to regulate the commercialisation of multidose pharmaceutical specialties susceptible to deterioration when opening the package.
INTEGRATION OF A ROBOT INTO THE EXISTING WORKFLOW OF THE CYTOSTATIC DRUGS DEPARTMENT IN A HOSPITAL PHARMACY (submitted in 2019)
Pdf

European Statement
Production and Compounding
Author(s)
Swantje Eisend, Herwig Heindl, Karen Tiede, Sven Jirschitzka
Why was it done?
Definition of an organisational structure for the best implementation of APOTECAchemo technology in the UKSH hospital pharmacy workflow
What was done?
The implementation of robotic systems for aseptic compounding cytotoxic drugs requires a specific workflow organisation in the hospital pharmacy to ensure an optimal combination of manual and automated production as well as the effective use of the technology. Since 2017, the APOTECAchemo robot has been installed in the hospital pharmacy and one of the first objectives was to create an organisational structure that would allow successful integration of the system into the existing workflow of the cytostatic department.
How was it done?
The pharmacy has carried out an analysis to identify the active substances that can best be transferred into automated production based on 4 main points: • Pharmaceutical form of the active ingredients: liquid or powder; • Average of vials needed for the compounding of one preparation for each active ingredient; • Average of ml of medication required for the compounding of a preparation associated with each specific active ingredient; • Robot compounding speed. In addition, the pharmacy has also tried to identify the optimal organisation of personnel and daily workflow for the automated compounding. The effectiveness of these measures and the work organisation defined have been evaluated through an intensive compounding week in April 2018.
What has been achieved?
The analysis of the active substances and the data collected during the “Robotic Intensive Week” showed the following results: • 42% of the total production was operated by APOTECAchemo; • 87% of active ingredients was handled by APOTECAchemo; • average of 60 preparations per day (with an actual working time of 5 hours); – average of 12 preparations per hour.
What next?
The study shows that the planning and organisation of the workflow plays a central role in the implementation of a robot solution in a hospital pharmacy. Through the work carried out, the hospital pharmacy has successfully integrated automated and manual production.
IMPLEMENTING THE PRODUCTION OF STERILISED SYRINGES IN THE HOSPITAL: IMPROVING MEDICATION SAFETY AND SAVING HEALTHCARE COSTS
Pdf

European Statement
Patient Safety and Quality Assurance
Author(s)
Karin Larmene-Beld, Rommert Wijnsma, Gerrit de Weerd, Maarten Postma, Erik Frijlink, Katja Taxis
Why was it done?
Medication administration errors are common in hospital practice. Meta-analyses suggest that about 10% of administrations are erroneous, with much higher error rates occurring during intravenous drug administrations. It has been demonstrated that 21% of the errors can be eliminated when prepared syringes are used. Many countries struggle with the problem of optimising the process of safe parenteral medication in hospitals. Different guidelines across countries outline how preparation of parenteral medication in the clinical environment should be done. Recently the Council of Europe published a resolution about preparation of medication which encourage the supply of ready-to-administer products by the pharmacy. Moving the activities of preparation of medication from the clinical environment to the pharmacy requires investments in pharmacy equipment but will result in efficacy, better quality and reduction in preparation medication errors in the hospital.
What was done?
Development and implementation of sterilisable plastic syringes produced in the hospital pharmacy for large-scale production of ready-to-administer products.
How was it done?
A new development in this area are ready-to-administer pre-filled sterilised syringes (PFSS) produced by the pharmacy. PFSS are produced on stock under GMP conditions by the hospital pharmacy using (semi) automatic filling and closing machines whereby quality and safety are embedded in the whole process of manufacturing. A total cost of ownership analysis is performed showing PFSS prepared in the hospital pharmacy yielded cost savings compared to conventional preparation on the ward. The process of production, filling, closing and sterilisation has been validated using newly acquired equipment. With the introduction of the cyclic olefin polymer (COP) syringes a new type of primary container is implemented in the pharmacy. To ensure patient safety and product quality a science- and risk-based strategy has been developed for testing extractables and leachables to qualify the new container as primary packaging material.
What has been achieved?
Introducing PFSS is cost saving for the healthcare system:– COP syringes are suitable as primary packaging material; –enhancement styles for better readability of labels are established; and – already, 15 products are validated and available for use in the hospital.
1. KHM Larmené-Beld KHM, Touwen-Spronk J, Luttjeboer J, et al. A cost minimization analysis of ready-to-administer pre-filled sterilized syringes in a Dutch hospital.. Submitted for publication in Clinical Therapeutics.
2. Larmené-Beld K, Kuiper A, van Berkel S, et al. A science- and risk-based strategy to qualify sterilized prefilled syringes as primary packaging material in a hospital pharmacy. Abstract submitted for 24th EAHP Congress.
3. Larmené-Beld KHM, Kim Alting E, Taxis K. A systematic literature review on strategies to avoid look-alike errors of labels. Eur J Clin Pharmacol 2018 74:985–93.
What next?
Introducing more drugs as ready-to-administer products. Optimising the label of ready-to-administer syringes to avoid look-alike errors based on the results of the review.
HOW TO HANDLE ACTIVE AND PLACEBO DRUGS FOR A CLINICAL TRIAL IN THE PRODUCTION SYSTEM CATO IN ORDER TO SECURE THE BLIND AND TO ENSURE THE EXACT SAME PREPARATION OF ACTIVE AND PLACEBO PRODUCTS
Pdf

European Statement
Production and Compounding
Author(s)
Kirsten Lykke Vorbeck
Why was it done?
When preparing treatments for blinded clinical trials it is very important to make sure that it is not possible to distinguish between the active and the placebo dose, as this may lead to unblinding of the treatment and thus jeopardise the results of the trial.
What was done?
The purpose was to find solutions for how to handle active and placebo drugs in the production system CATO to ensure they would end up being identical when prepared.
How was it done?
Before preparing a drug using CATO the drug must be registered in the system with all of its data. It is not possible to have two different sets of data for one drug. CATO records detailed documentation of what is being done during preparation and it is not possible to pretend to pick one drug and then grab another instead. Also, the label is printed automatically so it will show exactly what was prepared. We decide on a common name for the active/placebo and register both of these in the system under that name so that they will be prepared in exactly the same way and appear identical on the label but are still distinguishable in the batch documentation. We name the drug ‘Protocol name Active substance/placebo’ and register the stock of both active drug and the sodium chloride solution that is used as placebo under that name. We will also stock vials of NaCl for this purpose next to the drug it is being placebo for, and NaCl can be prepared pretending it has the density of the drug. CATO will think they are the same drug but they have been registered with their very different batch numbers, maybe with a NaCl after the number of that, so it is always possible to see what was actually being prepared.
What has been achieved?
Our doses of active and placebo are indistinguishable. Labels are the same and, for example, withdrawal into a syringe and insertion of a needle into the port of the infusion bag will be done in the same way.
What next?
These very simple routines can be used anywhere for the preparation with CATO and possibly also with other systems.
DEVELOPMENT OF NEW PRODUCTION WHEN NEITHER PACKAGING NOR SOME OF THE RAW MATERIALS CONFORM TO EUROPEAN STANDARDS
Pdf

European Statement
Production and Compounding
Author(s)
Katrine Bødker Rubach-Larsen, Anne Rungø, Anette Eskildsen, Lone Skovhauge
Why was it done?
A research team at the MR Centre (MRC2) wished to set up the production of Pharmacy Kits, but had no prior experience of, or licence to, manufacture drugs. Thus, the hospital pharmacy was asked to participate in the development of such production.
What was done?
A new MR-scanning technology, hyperpolarisation, for the quantification of metabolic processes with an extremely high sensitivity enables physicians early detection of treatment effects in, for example, cancer and diabetes. A so-called Pharmacy Kit is used in the hyperpolarisation process and consists of a specially designed packaging with tubes, vessels and filters containing the contrast agent and buffer solutions. The objective for the hospital pharmacy1 was to manufacture Pharmacy Kits complying with Good Manufacturing Practice (GMP), though neither packaging nor two of the raw materials conformed to European standards.
How was it done?
The MRC research team presented the hospital pharmacy with the desired combination of compounds and the packaging required for Pharmacy Kit production. The task for the hospital pharmacy was then to set up a manufacturing process that met these requirements and complied with the guidelines for GMP. A production complying with GMP was developed in close collaboration with the MRC and an ongoing contact with the Danish Medicines Agency. During the process the hospital pharmacy carried out its own microbiology test in order to determine if, and for how long, the non-CE-marked packaging could store the contrast agent and buffer solutions. Risk assessment of the raw materials not found in the European Pharmacopeia were conducted. The method investigated by the MRC already takes place at a few other places in and outside of Europe. Experiences from these production sites were implemented and expanded with process optimisation, and specially designed equipment for the production.
What has been achieved?
Due to a strong inter-professional collaboration between the MRC and the hospital pharmacy and due to qualified risk assessments, it was possible to set up a production of Pharmacy Kits according to GMP.
What next?
When researchers contact hospital pharmacies with new ideas, we have to be willing to work with GMP in a different way by applying knowhow and risk assessments in order to ensure developments within the healthcare system.
1. Hospital Pharmacy Central Region, Production, Aarhus, Denmark.
2. MR Centre, Aarhus University Hospital, 8200 Aarhus N, Denmark
IMPROVING THE CONTINUITY OF CARE IN CASE OF EXTRATEMPORANEOUS MEDICINES FOR CHILDREN
Pdf

European Statement
Clinical Pharmacy Services
Author(s)
Stefanie Sauer, Michael Ober, Jürgen Backhaus, Torsten Hoppe-Tichy
Why was it done?
Patients of the Children’s Hospital at the Heidelberg University Hospital are regularly supplied with extratemporaneous medicines from the hospital pharmacy. This often leads to issues in continuity of care in the outpatient setting as patients are required to access ongoing treatment through local pharmacies, which in turn must develop the formulations and procure the necessary raw materials. Therefore, it is not uncommon for interruptions in patients’ therapy to occur.
What was done?
The aim was to improve continuity of care by discussing the medication with the responsible pharmacy before the patient was discharged. Allowing missing raw materials to be procured and clarify any uncertainty about the prescription.
How was it done?
We designed a document that is available on the Intranet. While the child is still on the ward the discharge medication should be noted. The parents had the opportunity to indicate a retail pharmacy of their choice, preferably near the place of residence. This document could be sent to the hospital pharmacy. A hospital pharmacist contacted the specified pharmacy to discuss the extemporaneous medications before the child was discharged. If necessary, the pharmacist can forward the hospital pharmacy manufacturing instructions. Furthermore, the compositions plus further information were then made available on the homepage of the pharmacy in an area to which only experts have access. A telephone number on the hospital pharmacy homepage is available for queries, including those about the formulations.
What has been achieved?
In the discussions with the retail pharmacies, the colleagues were very pleased and grateful about the service provided by the hospital pharmacy. They saved time in preparing patients’ prescriptions. Concerns or doubts were cleared up at an earlier stage of the discharge process, leading to the patient receiving their medicine on time.
What next?
Provision of the document and manufacturing instructions on the homepage serve as a valuable aid for ensuring that the outpatient therapy functions smoothly. It is important that the information is kept current. In the future, further information will be linked to the homepage in the hope of reducing the number of incoming telephone enquiries.
QUANTIFICATION OF WAITING TIME REDUCTION IN OUTPATIENT SETTING USING ASSISTED SYSTEMS IN AN AUTOMATED ONCOLOGY PHARMACY
Pdf

European Statement
Production and Compounding
Author(s)
Jemos Costantino, Martina Milani, Mariantonietta Piccoli, Mara Provenzi, Paola Paochi, Ilaria Clerici, Cinzia Lucia Ursini, Claudio Colosio, Fabrizio Mastrilli, Emanuela Omodeo Salè
Why was it done?
In outpatient setting, WT between medical visits and administration is strongly conditioned by time needed for preparation. We needed to reduce our WT caused by the use of an automated system by ensuring the same standards of quality control checks and traceability, not achievable with manual preparation.
What was done?
We introduced an assisted system for chemotherapy preparation, with a gravimetric and barcode verification. We started to switch part of preparations previously prepared by an automated system to this assisted system. We performed an analysis to measure the impact of a different strategy in preparing chemotherapy on patients WT.
How was it done?
Time needed for preparation was monitored in the first trimester of 2016, where drugs were prepared using an automated system or manually, and compared to the first trimester in 2017, when we introduced the assisted system.
In the first period we used a “WT optimization” criteria in selecting the preparing technology, while in the second period we decide to use a “risk based” criteria.
Risk based criteria consists of selecting the automated system for cytotoxics, assisted system for antibodies and low risk drugs and manual procedure when no other options are available.
In order to evaluate bias introduced by the risk based selection of different drugs, we performed a contest comparing preparation times of a defined sequence of representative preparations typologies. Three technicians are involved in order to reduce human factor impact.
What has been achieved?
Average WT (AWT) in the first period was 1h36m and median WT (MWT) was 1h22m (sample = 2365 preparations in 3 months). AWT in the second period (sample = 3437 preparations in 3 months) was 1h17m (-19,79%) and MWT 1h1m (-25,61%). The percentage of therapies dispensed after 2 hours waiting decreased by 55,69%. WT was stratified by preparation technology (assisted system: AWT =50m; MWT=44m – automated system: AWT=1h26m; MWT=1h07m).
The contest results were (average of three series) : manual preparation 15m19s; assisted 26m42s; automated 1h14m3s.
What next?
Assisted systems are able to guarantee quality standards for patients similar to automated ones, but with an important reduction in WT when compared with an automated one and an improvement in traceability compared to the manual procedure.
IMPLEMENTING A NATIONAL PORTFOLIO OF EXTEMPORANEOUS PHARMACEUTICAL PREPARATIONS USED IN DANISH HOSPITALS
Pdf

European Statement
Introductory Statements and Governance
Author(s)
Janne Jensen, Solvej Wandy Pedersen, Susanne Nørregaard, Karin Herkell, Anne Thestrup Nielsen, Anita Gorm Pedersen
Why was it done?
A group of hospital pharmacists representing all hospital pharmacies in Denmark have in a previous study identified and slimmed a national portfolio of extemporaneous pharmaceutical preparations used by Danish hospitals from a total of 2,754 preparations down to approximately 750 preparations being considered of clinical importance. Without a common overview of the national portfolio there will be initiated production of duplicates and almost identical products resulting in a large and inconsistent portfolio.
The purpose of this GPI was to make the national portfolio of extemporaneous pharmaceutical preparations accessible to all hospital pharmacists in Denmark and to implement a common procedure to evaluate preparations before adding them to the national portfolio to avoid duplets and obsolete products.
What was done?
A common national procedure for adding new preparations to the national portfolio was developed and implemented to avoid duplets and to ensure a uniform quality and appropriate risk assessment of the preparations.
How was it done?
A national database was developed and tested. Each hospital pharmacy entered their own extemporaneous pharmaceutical preparations in the database. Also, the extemporaneous pharmaceutical preparations manufactured by community pharmacies and used in the hospitals were entered in the database.
One hospital pharmacist in each of the five regions in Denmark was appointed as gatekeeper for the national portfolio. A template for an application form for new preparations was developed. When a physician requests a new preparation the application form will be completed by the clinical pharmacist. It is forwarded to the gatekeeper who will evaluate the preparation before approving it as a candidate for the national portfolio.
What has been achieved?
430 extemporaneous pharmaceutical preparations from the hospital pharmacies are entered and quality approved in the database. 255 extemporaneous pharmaceutical preparations manufactured by community pharmacies were entered in the database.
A national group of five gatekeepers was formed, and the workflow for both the group and the individual gatekeeper was described and implemented at all Danish hospital pharmacies.
What next?
The GPI provides an easy-accessible overview of the national portfolio of extemporaneous pharmaceutical preparations, releasing production time and resources at the manufacturing pharmacies.
IMPLEMENTING NEW CHEMOTHERAPY COMPOUNDING WORKFLOW USING SEQUENTIAL PDSA CYCLES TO INCREASE PRODUCTION CAPACITY, REDUCE WAITING TIME, IMPROVE RESOURCES UTILIZATION, AND MINIMIZE THE RISK OF ERRORS
Pdf

European Statement
Production and Compounding
Author(s)
A Elsheashaey, A Elshishiny, A Orabi, A Almutairi, A Aboulwafa, H Alobaid, F Dashti, D Saeed, R Yassin, M Salama
Why was it done?
Kuwait Cancer Control Center (KCCC) is the only oncology hospital in Kuwait. Chemotherapy Preparation Unit (CTPU) was unable to meet the increased orders; causing delivery delay and more patients’ waiting time. Moreover; rework and more waste due to defective and faulty processes of current workflow resulting in frequent incident reports of wrong final products dispatched.
What was done?
Shifting to a systematic multi-step production workflow to increase compounding capacity, minimize risk of errors, reduce processing time, and maximize utilization of integrated technological resources.
How was it done?
Using multiple PDSA cycles, a comprehensive educational and practical training was conducted, proceeded by staff rotation with newly trained team. Every three weeks a new pharmacist trained and assigned to CTPU. Raw materials stores were rearranged for better accessibility and diminishing unnecessary staff movement. A staging step as the first independent double-check before the start of compounding, and for assembly of raw materials and supplies required for compounding. A verification Step as the second independent double-check upon compounding, using bar-code scanners, touchscreens and cross-checking with the chemotherapy order to assure the quality and integrity of the finished product. Production workload were restructured over three parallel line of manual stations and one automated preparation unit. Pharmacy Information System (PIS) screens were customized to give a first and second audio-visual alarms after 30 and 45 minutes of transcription time respectively. Chemotherapy sessions appointment system were established to assess the daily chemotherapy compounding needs from CTPU in advance with an incremental increase of production capacity to reach 100~120 patients/day or 180~200 preparations/day.
What has been achieved?
Number of preparation compounded by CTPU was increase by 8%, where more than 43% of preparations were validated to release in less than 30 minutes and approximately 88% of preparations were delivered in less than 45 minutes. Number of preparation by automation was increased by 82%, Furthermore, all production incidences has been completely eliminated after full implementation of final verification and validation step.
What next?
The new workflow has increase the workload capacity with less production errors and zero incident reports. Patient experience was improved by comparable preparation time to other international Pharmacy Workload Unit and average time required per patient visit.