Medical supply vending machines – a direct-to-patient distribution method that offers flexibility to outpatients
European Statement
Selection, Procurement and Distribution
Author(s)
Louise Refsgaard, Linda Skovsted, Nina Bøggild
Why was it done?
The medical supply vending machines were implemented during 2021 as a way of direct-to-patient distribution of medicine with more flexibility. The aim was to offer 24-hour access to collect medicine at a location that suits the patient, e.g. close to the patient’s home.
What was done?
Medical supply vending machines were implemented in the Capital Region of Denmark. The vending machines allow patients to collect their medicine whenever and wherever it suits them. It is the patient’s healthcare professional that controls and orders the medicine. The hospital pharmacy staff consults the prescription and labels, dispenses and records the medicine and places it in the vending machine for collection.
Patient and staff satisfaction was surveyed.
How was it done?
The implementation of this new direct-to-patient distribution method was carried out by the Capital Region Hospital Pharmacy in close collaboration with the region’s hospitals and outpatient departments. Installing the machines was fast but a full implementation requires that the clinical staff rethink their practice and accept that dispensing is no longer their responsibility. This has been the biggest obstacle along with creating patient safe procedures.
What has been achieved?
7 medical supply vending machines were installed centrally in hospitals in the Capital Region of Denmark. The machines are now used to distribute medicine to some of the region’s outpatients.
The patient satisfaction survey showed that the patients are very satisfied with the vending machines: 100 % are either ‘highly satisfied’ (86 %) or ‘satisfied’ (14 %) with the new service, and 97 % would like to use it again. The staff was also satisfied with the new service.
Additionally, the quality of medicine dispensing is increased due to hospital pharmacy staff dispensing the medicine rather than nurses.
What next?
In order to offer flexibility to patients and increase the quality of dispensing of medicine, we aim to increase the number of patients that collect their medicine from the vending machines by using the current machines in their full capacity and installing more machines. We also aim to collaborate with Denmark’s other 4 regions, so that patients, who are treated outside their home region, can collect their medicine in a vending machine closer to their home.
OPTIMIZATION AND CENTRALIZATION OF THE HANDLING CIRCUIT OF HAZARD DRUGS FROM THE PHARMACY SERVICE
European Statement
Clinical Pharmacy Services
Author(s)
Mireia Iglesias Rodrigo, Júlia Pardo Pastor, Alba Manzaneque Gordon, Cristina Sangrador Pelluz, Núria Meca Casasnovas, Clara Sebastián Carrasco, Fernando Salazar Gonzalez, Gemma Garreta Fontelles, Jordi Nicolás Picó
Why was it done?
Due to the risk posed by the handling of Hazard Drugs (HD) in the healthcare field, it is necessary to implement circuits that guarantee the professional’s safety.
What was done?
Create an internal classification of HD based on the NIOSH List of Hazard Drugs in Healthcare Setting 2020, to optimize the circuit of its handling from its receiving to its administration.
How was it done?
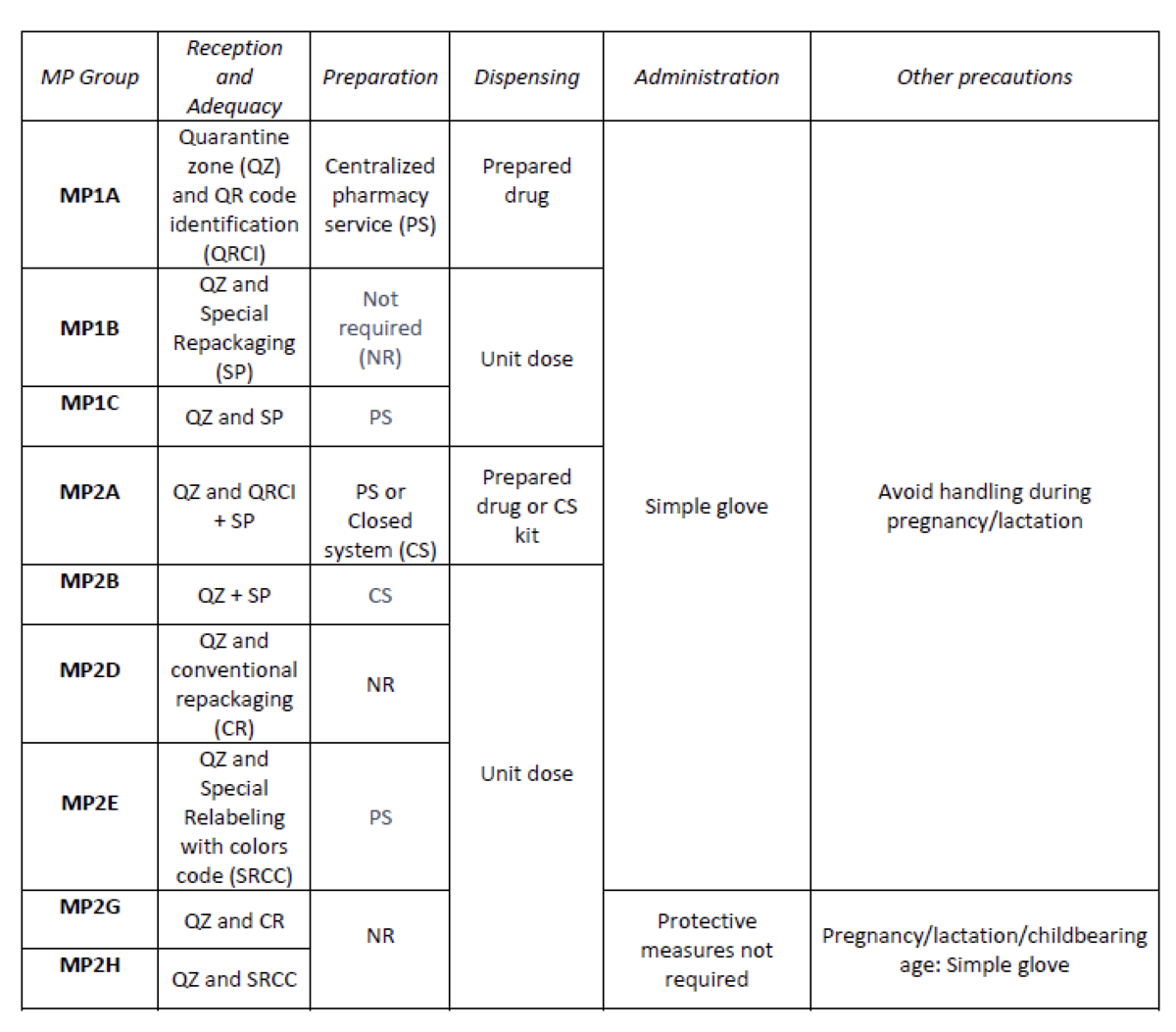
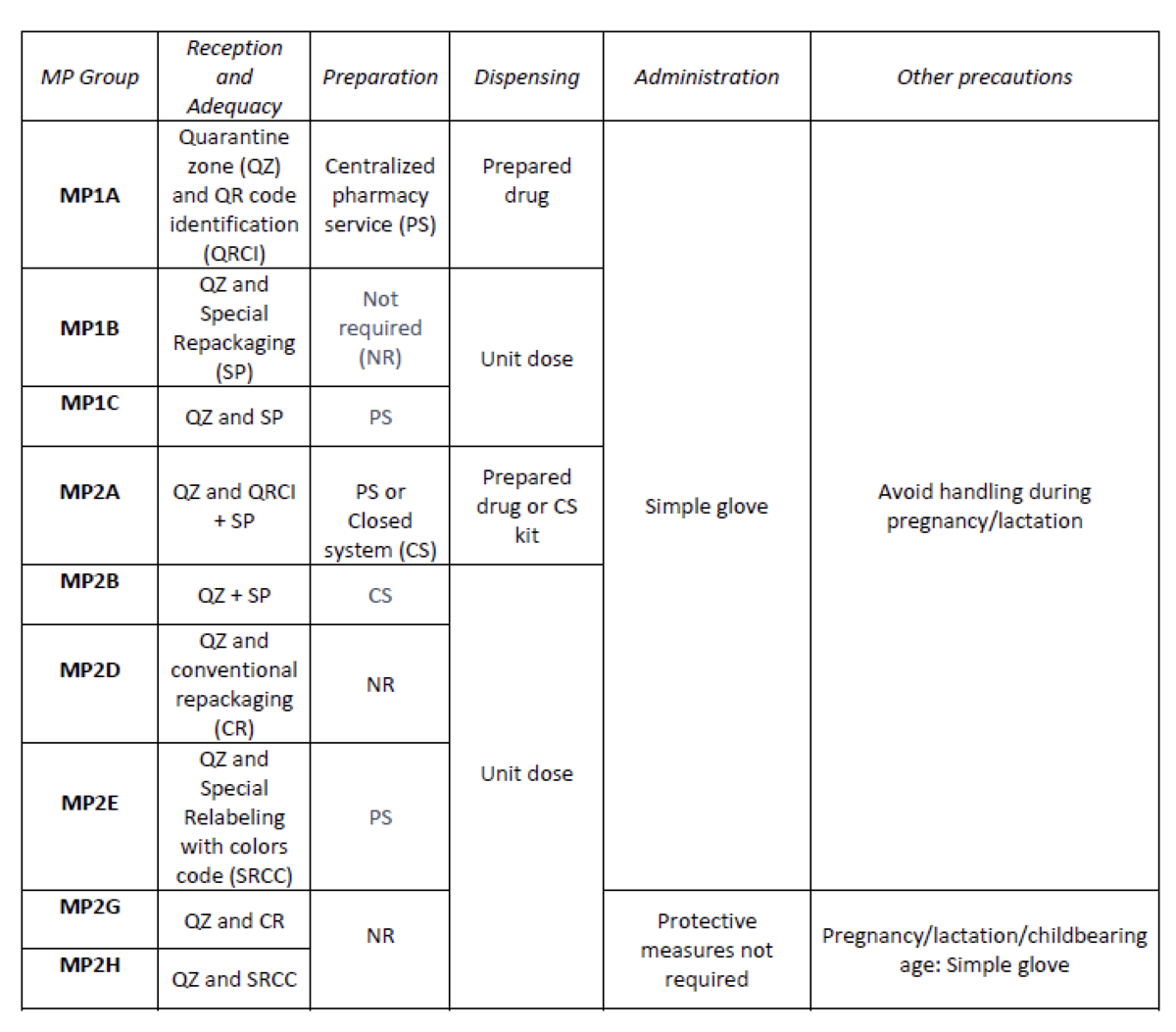
Considering the HD included in the Pharmacotherapeutic Guide (PTG) of our center, the stages of reception and adaptation/preparation/dispensing/administration and other precautions were analyzed.
Categories were established, analyzing the needs of each stage according to: NIOSH level of danger, setting (inpatient/outpatient), pharmaceutical form, commercialized pharmaceutical specialties or available alternatives, and material/personal resources.
Prior to its implementation, e-learning training was carried out for the healthcare professional involved.
What has been achieved?
A total of 25.3% (379/1498) of the pharmaceutical specialties included in PTG were HD. Thirteen HD groups were identified. Due to the fact that in the outpatient setting the drug is dispensed to the patient in its original container, the actions implemented were only carried out for inpatients, representing these 9/13 of described groups. The established training was carried out by the 89% of professionals. Proposed measures for HD are summarized in Table 1.
What next?
Monitoring and evaluation of the circuit
EXPANDING OPPORTUNITIES FOR PHARMACISTS IN ONCO-HEMATOLOGIC CLINICAL TRIALS: DESIGN AND IMPLEMENTATION OF THE OUTPATIENT SERVICE MODEL
European Statement
Clinical Pharmacy Services
Author(s)
Eugenia Serramontmany Morante, Patricia Garcia Ortega, Lorena Garcia Basas, Pablo Latorre Garcia, Pilar Rovira Torres, Laura Maños Pujol, Isabel Cidoncha Muñoz, M. Queralt Gorgas Torner
Why was it done?
The provision of outpatient oncology services by pharmacists is still limited, but it is an emerging role. It can add value while increasing the quality of patient care required, maximizing the likelihood of achieving positive outcomes and thus improving the patient’s quality of life. It is important to incorporate clinical pharmacists into outpatient clinics to ensure the safe use of investigational drugs and guarantee the best treatment for the patient.
What was done?
The oncology clinical trials pharmacy team initiated an outpatient clinic at a tertiary hospital. This enabled review of patients’ medications, monitoring of interactions, appropriate oral chemotherapy counseling, design of medication diaries and instructions, discussion of side effects, as well as other dietary and daily living recommendations.
How was it done?
A multidisciplinary team was formed: pharmacy, medical, nursing, ancillary and administrative staff, to discuss circuits and strategies to address outpatient pharmacy clinic.
The pharmaceutical care program was implemented gradually during 6 months, first in phase I, then phases II and III clinical trials.
Factors including appointment scheduling, patient prioritization, clinic room availability as well as detailed definition of pharmaceutical activity were discussed, in order to have a standard procedure for all patients included in a clinical trial.
The group continued to meet weekly to further discuss the progress of the pharmaceutical care program and any obstacles and unforeseen events.
What has been achieved?
Medication has been dispensed to 8447 patients in the outpatient pharmacy, of which 1172 patients have been attended by the clinical pharmacist during the first 8 months (January-August 2021) of the programme’s implementation.
Pharmaceutical care at the first day of treatment has been provided to 275 patients to explain how to take the treatment and resolve doubts. The concomitant medication of 312 patients has been reviewed for the screening and 425 telephone queries about concomitant medication have been resolved.
What next?
The evolutionary change in cancer care along with the increase in the number of clinical trials and its complexity will emphasize the need to include the oncology pharmacist in the cancer care team. The role of a clinical pharmacist is vital to ensure the safety and controlled use of the drug, ensuring the best possible outcomes.
Impact of introducing a Unit Dose blister service in an Austrian hospital
Pdf

European Statement
Patient Safety and Quality Assurance
Author(s)
Theodora Steindl-Schönhuber, Gittler G.
Why was it done?
Medication dispensing is a time-consuming, labour-intensive, error-prone process in the daily routine on the wards. The project was triggered by the tight personnel situation during the Coronavirus pandemic: In November 2020 three wards with COVID-19 patients (91 beds) were integrated into our Unit Dose blister service to assist the nursing staff. A multidisciplinary effort (management, IT-department, doctors, nursing staff, pharmacy holding a GMP-manufacturer´s certificate) and long-established electronic patient records including medication data enabled fast realisation.
After transformation back to a chirurgical, an internal and a geriatric ward the service was continued and extended to the neurological unit (49 beds) due to positive feed-back. We wanted to study the observed positive effects of Unit Dose supply in more detail.
What was done?
In our hospital medication distribution has been switched from manual dispensing by ward staff to automated Unit Dose blister packaging by the pharmacy. Our study investigates the impacts of this change on medication safety, staff satisfaction, time and drug resources.
How was it done?
The percentage of pharmacy-blistered drugs, time gain for nursing staff, employee satisfaction, medication consumption and erroneous blister fillings were investigated.
What has been achieved?
Unit Dose in hospitals is not standard for many countries and is so far unique in Austria. Therefore, we would like to share our experiences and findings with our colleagues: Solid, oral dosage forms could be supplied by 99% via Unit Dose. Time for manual drug dispensing was reduced by 75%. A survey showed high employee satisfaction with the supply process as well as the quality and correctness of the blisters. Consumption of blisterable drugs and stocks on the ward were reduced by 44% and 78%, respectively. Errors in blister fillings in our setting amount to 0,006%. When compared to literature references on error rates for manual medication dispensing (up to low double-digit rates), patients benefit from increased drug therapy safety. On the basis of these results our initiative was granted the Austrian Patient Safety Award 2021 in the field of medication safety.
What next?
We plan to extend Unit Dose to the remaining wards and to investigate patient satisfaction with the blisters, cost-efficiency and distribution of high-cost medications.
Croatian hospital pharmacists managing earthquake(s) medical consequences during lockdown(s)
European Statement
Clinical Pharmacy Services
Author(s)
Mirna Momcilovic, Anita Simic, Petra Turcic
Why was it done?
Croatia was hit by 2 big earthquakes in 2020, both happened just right after 1st and 2nd lockdown due to high number of COVID-19 cases. Since most of the hospitals were strategically built on the hills, it was more destructive for them. It also hit a number of community pharmacies responsible for drugs supply to specific areas in the country. There was no electricity, no heating, no drugs supply, no fridge to store drugs, for days, so quick back-up plan was needed to provide minimal healthcare.
What was done?
Croatian hospital pharmacists organised a temporary pharmacy in a tent, filled it with drugs and medical products donated from community pharmacies, hospitals and wholesalers from Croatia and other European countries and started supplying patients with it.
How was it done?
It was modified way of dispensing, without prescription because there was no doctors and no place to prescribe it, based on patient’s medical documentation, if available, and patient’s medication history according to what patient said only. Pharmacists needed to use their knowledge about dosing, duration of action – difference between immediate release or modified release formulations, possibility of splitting tablets into equal parts to get the needed dose and, most important, substituting drugs from the same pharmacologic class (ex. switching from one inhaler for treatment of asthma containing ICS + LABA to another one that was available at the moment), taking into consideration patient’s needs and avoiding drug to drug interactions. Pharmacists provided patients with OTC drugs, free of charge, followed by an advice of how to use it. Non having prescription problem was solved afterwards by Croatian Health Insurance Fund. Also, all the supply of vaccine against COVID-19 available in Croatia at that point, was sent to an area hit by the earthquake. Vaccination was done by doctors, and pharmacists assisted by supplying them with all the equipment needed (needles, alcohol, cotton wool, etc.).
What has been achieved?
Patients were supplied by all the drugs/medical products needed in the first, critical week after an earthquake.
What next?
Following the Croatian example of handling an earthquake situation, there is an idea of organising a medical crisis team, would include pharmacist, in each European country.
Parenteral Nutrition Waste Reduction Initiative
European Statement
Selection, Procurement and Distribution
Author(s)
Marie O Halloran, Siobhán Nestor
Why was it done?
This project was undertaken in reaction to an evolving healthcare environment. It was important to identify patterns to improve the efficiency of the purchasing and dispensing process, and to ensure that PN levels held in the Pharmacy Department respond to requested use within the hospital. The aim was to reduce the amount of PN bags expiring with associated cost savings and waste avoidance.
What was done?
The Pharmacy Department is responsible for dispensing Parenteral Nutrition (PN) in the Mater Misericordiae University Hospital (MMUH). PN is purchased from a third party manufacturer. On receipt by the hospital, the standard PN bag has an expiry date of approximately 60 days. Given the need for rapid turnover of PN to avoid expiration and wastage, coupled with the rapidly changing healthcare landscape, the pharmacy instigated a review of the factors contributing to PN waste and opportunities to improve and optimise the associated processes.
How was it done?
• PN Stock Holding Review
Due to surgery volumes and the complexity of the patient cohort in MMUH, the Pharmacy Department are required to hold a stock of PN bags for patients to access in a timely manner. The agreed levels of stock held was identified as a key target to reduce waste. The quantity of each stock bag held was reviewed between Pharmacy and Clinical Dietetics utilising recent usage pattern reports. This resulted in removing certain bags from MMUH stock entirely and reducing the stock quantity of slow-moving bags.
• Improved communication to dietitians
A standard email template was devised to send to all stakeholders, by a Dispensary Pharmacist, detailing the stock of each bag on hand and highlighting bags which would expire in the following two weeks. The Dietitians endeavour to utilise this short-dated stock for suitable patients to avoid waste.
What has been achieved?
Through the improvement initiatives outlined above, PN waste reduced by 74% (117 bags versus 31 bags) in Q1-Q3 2021, compared to the same period in 2020. This resulted in a considerable associated cost saving.
What next?
We will continue our collaborative work with Clinical Dietetics to further reduce PN waste. We now have a dynamic stock management process, which responds to the changing patient cohort in MMUH.
Case-study: Pharmaceutical teleconsultation using a mobile application
European Statement
Clinical Pharmacy Services
Author(s)
Joana Russo, Maria João Ribeiro, Humberto Gonçalves, Joana Ribeiro, Silva Cristina, António Gouveia
Why was it done?
In our country the oncology medication for ambulatory patients is dispensed by the hospital pharmacist (HP). Due to several aspects (i.e., COVID-19 pandemic) the process of distribution of said medication has changed in that the HP and the patient no longer meet face to face (Drive-thru systems, proximity projects in which the medication is sent to a nearby pharmacy of the patients living area). A tool was required that enabled the HPs to continue to monitor the relevant clinical aspects (patient education; medication adherence (MA), drug interactions (DI) and adverse events (AE) evaluation).
What was done?
We used a mobile application (App) to conduct the pharmaceutical evaluation of clinical aspects that need to be considered when dispensing oncology medication.
How was it done?
In collaboration with the Information Technologies department of our hospital, an App was developed. It integrates the patient’s hospital prescriptions and their answers to an adaptive query that identifies cases that need further clinical data We selected a specific drug (ibrutinib) and developed an algorithm that presented the extended questions accordingly. The App was announced to patients that required hospital medication and wanted to receive it through an alternative method of distribution.
What has been achieved?
In little over a year, a total of 1720 requests were received (668 patients). The algorithm was successful in differentiating patients whose evaluation needed to include additional clinical information. In 22 requests, further data was automatically gathered (9 patients) enabling us to evaluate MA, DI and AE. These teleconsultations do not require additional professionals (ie an assistant to register the request) nor a compatible time slot for a pharmacist-patient phone call.
What next?
The results showed that the concept of pharmaceutical teleconsultations through an App is viable and we intend to extend its range to other drugs and to dissociate the teleconsultation from the dispensing request. This approached also showed that proximity between HP and patients was positively affected allowing patients to consult their hospital pharmacist whenever they need to and wherever the patient was.
IMPLEMENTATION OF AN APPOINTMENT MANAGEMENT MODULE APPLIED TO THE OUTSIDE PATIENT AREA
European Statement
Patient Safety and Quality Assurance
Author(s)
JUDIT PERALES PASCUAL, ANA PÉREZ LÓPEZ, HERMINIA NAVARRO AZNAREZ, ELENA HERRANZ BAYO, MARIA PEREZ MORENO, CARLOS-IGNACIO DIAZ CALDERON HORCADA, Mª REYES ABAD SAZATORNIL
Why was it done?
In 2019 the UPEX attended a large volume of patients without a scheduled appointment, long waits were generated and the pharmacotherapeutic follow-up was complicated. The purpose was to implement an appointment management module to avoid crowds, excessive waiting times, allowing better organizational management of care and knowledge of patients in each type of consultation.
What was done?
An outpatient is a patient who goes to the outpatient unit of their Hospital Pharmacy Service to collect a drug for hospital use/diagnosis or foreign drug (it will be administered without health personnel intervention).
An appointment management system was implemented in accordance with the objectives of the SAMPA project (Service for Registration and Promotion of Adherence to Medicines for Elderly Patients), included in the European STOPandGo project.
How was it done?
Creating a cross-cutting system for the entire clinical circuit from prescription to dispensing involved a great deal computer involvement. Although it began to be used in November 2018, it was not used by the mostly part of prescribing doctors until the end of 2020.
Now, when the patient leaves medical consultation, he/she will go to the pharmacy and will be seen by a pharmacist. Besides, the program will propose a return appointment when it calculates that the patient has a week’s worth of medication, thus preventing the patient from running out of medication. The pharmacist will decide if the patient needs pharmacotherapeutic follow-up.
What has been achieved?
In 2019, 5 services cited patients while in 2020 it was 14; the percentage of patients attending pharmacy cited increased from 73.2%(2019) to 79.4%(2020).
Currently, the pharmacist knows in advance which scheduled patients he has and can establish a better organizational care management and determine in advance if the patient needs a close pharmacotherapeutic follow-up. Additionally, with this system an average waiting time of 03:55min was achieved (in 2019 appointments with waits >30min were recorded).
What next?
The implementation of the appointment management system has made possible to achieve better organizational management of care,avoid crowds,excessive waiting times, and provide better patient care and pharmacotherapeutic follow-up. The proposed solution can be extended to other hospitals.
TELEPHARMACY PROGRAMME IN CHRONIC NEUROLOGICAL PATIENTS DURING THE COVID PANDEMIC
Pdf

European Statement
Clinical Pharmacy Services
Author(s)
ROSARIO MORA-SANTIAGO, JOSE-LUIS ORTIZ-LATORRE, ELENA SANCHEZ-YANEZ, ANGEL JURADO-ROMERO, ISABEL MOYA-CARMONA
Why was it done?
During the health alert caused by Covid-19, home delivery was quickly implemented in our country to reduce attendance at the Hospital Pharmacy Service (HPS) to obtain their medications.
In our HPS we transform home delivery into telepharmacy program (TP) with chronic neurological patients, who suffering pathologies that decrease their autonomy, with the purpose to optimize clinical outcomes and reduce the risk of contagion.
What was done?
The main purpose was to design a telepharmacy program (TP) undertstood as the provision of pharmaceutical care by pharmacists through the use of telecommunications to patients located at a distance. Telepharmacy services include patient follow-up and clinical service delivery. In our case, home delivery is also included.
How was it done?
We design the TP stratifying stable chronic patients (more than 6 months of treatment) by level of autonomy, physical distance to our Hospital and high risk (due to immunosuppressive treatment). Inclusion in the TP was proposed to patients with multiple sclerosis (MS) and aminotrophic lateral sclerosis (ALS).
Telepharmacy appointments were recorded and scheduled within the outpatient care activity, they were recorded in the patient’s medical history, as a pharmaceutical clinical follow-up, reviewing adherence, interactions and possible adverse events. Later, home delivery was made, through an external logistics company. Patients gave their consent to transfer personal data for home delivery.
Data collected were: sex and age, first or second line treatment in MS patients, pharmaceutical form (pill or syrup ) in ALS patients and number of total deliveries made.
What has been achieved?
We started on April 2020 with the program, six months later 56 patients were included, 48 with MS (total of MS patients attended by our HPS: 296) and 8 with ALS ( total of ALS patient attended by our HPS: 58). Median age: 45 years in MS group and 65 in ALS group. In MS group 37 patients received 1st line treatment and 10 second line. In ALS patients 6 received tablets and 2 syrup.
420 deliveries took place (average: 3,1 for patient).
What next?
The implementation of the TP was well accepted, avoiding longed displacement in patients with neurological pathologies. Our future target is to reach a greater number of patients that can be included in the program.
HOME DELIVERY SERVICE DURING COVID-19 PANDEMIC TO RHEUMATOLOGIC DISORDERS
Pdf

European Statement
Patient Safety and Quality Assurance
Author(s)
Ana Pelaez Bejarano, Maria de las Aguas Robustillo Cortes, Pilar Villar Santos, Olalla Montero Pérez, Ignacio Garcia Gimenez
Why was it done?
Rheumatologic disorders carry increased risk of infection compared with the general population, so facilitate access to hospital medications is of vital importance.
What was done?
On 14 March 2020, the Spanish government declared a state of alarm to deal with the spread of COVID-19. Medication dispensing protocols were immediately established to deliver drugs to patients who could not come in person to the hospital pharmacy department. These measures were designed to benefit citizens who, due to age or physical fragility, were more vulnerable to contagion. We had the collaboration of community pharmacies actively practicing during the COVID-19 pandemic and a logistics service, with no extra cost to the public healthcare system.
How was it done?
Between 30 March and 1 September 2020, a circuit was designed as follows: First, patient request the delivery service in the community pharmacy of their choice, which sending the request of each patient to college of pharmacists. Later, this institution sending of applications received from all pharmacies to hospital pharmacy. Here, the hospital pharmacist reviewed the patient’s electronic medical record, checking that the medication requested was appropriate, modifying it if deemed necessary (change of drug, dose, and so on). A pharmaceutical cooperative sending antirheumatic drugs to the community pharmacies. Finally, the community pharmacist who received the package checked the medication and, with the patient, reviewed and reinforced the information on the treatment.
What has been achieved?
587 patients were included: 211 rheumatoid arthritis, 173 psoriatic arthritis, 121 psoriasis and 82 ankylosing spondylitis. The delivery service enabled us to provide antirheumatic drugs to patients in their immediate environment through a service that was free for both the patient and the hospital pharmacy service. This contributes to guaranteeing the achievement of the pharmacotherapeutic objectives established for these patients.
What next?
Further action is needed to identify which groups of patients require more intensive pharmaceutical care and, therefore, who could benefit most from telepharmacy, and not only the delivery service.