The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
You can subscribe to receive the EAHP EU Monitor by email here.
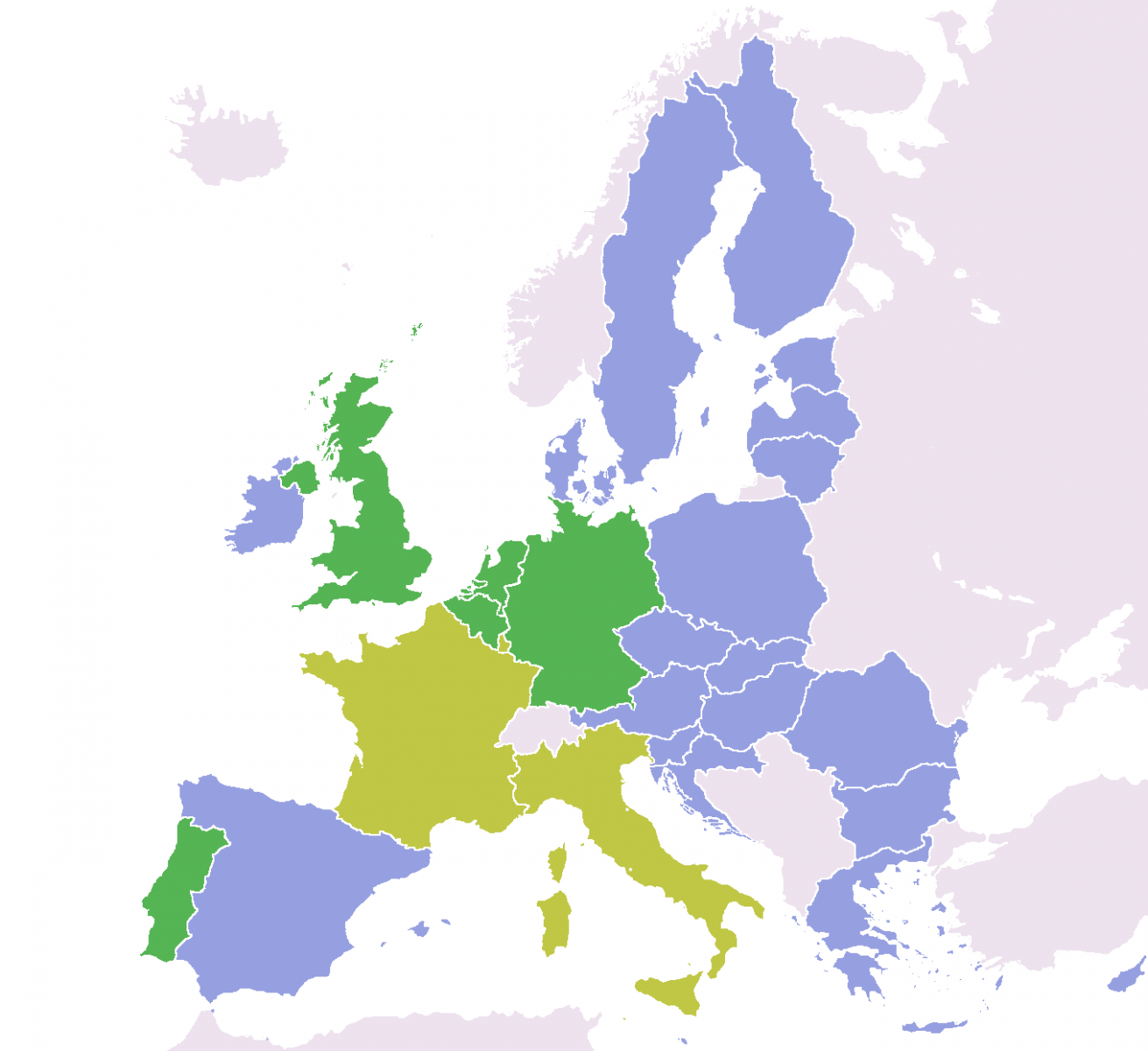
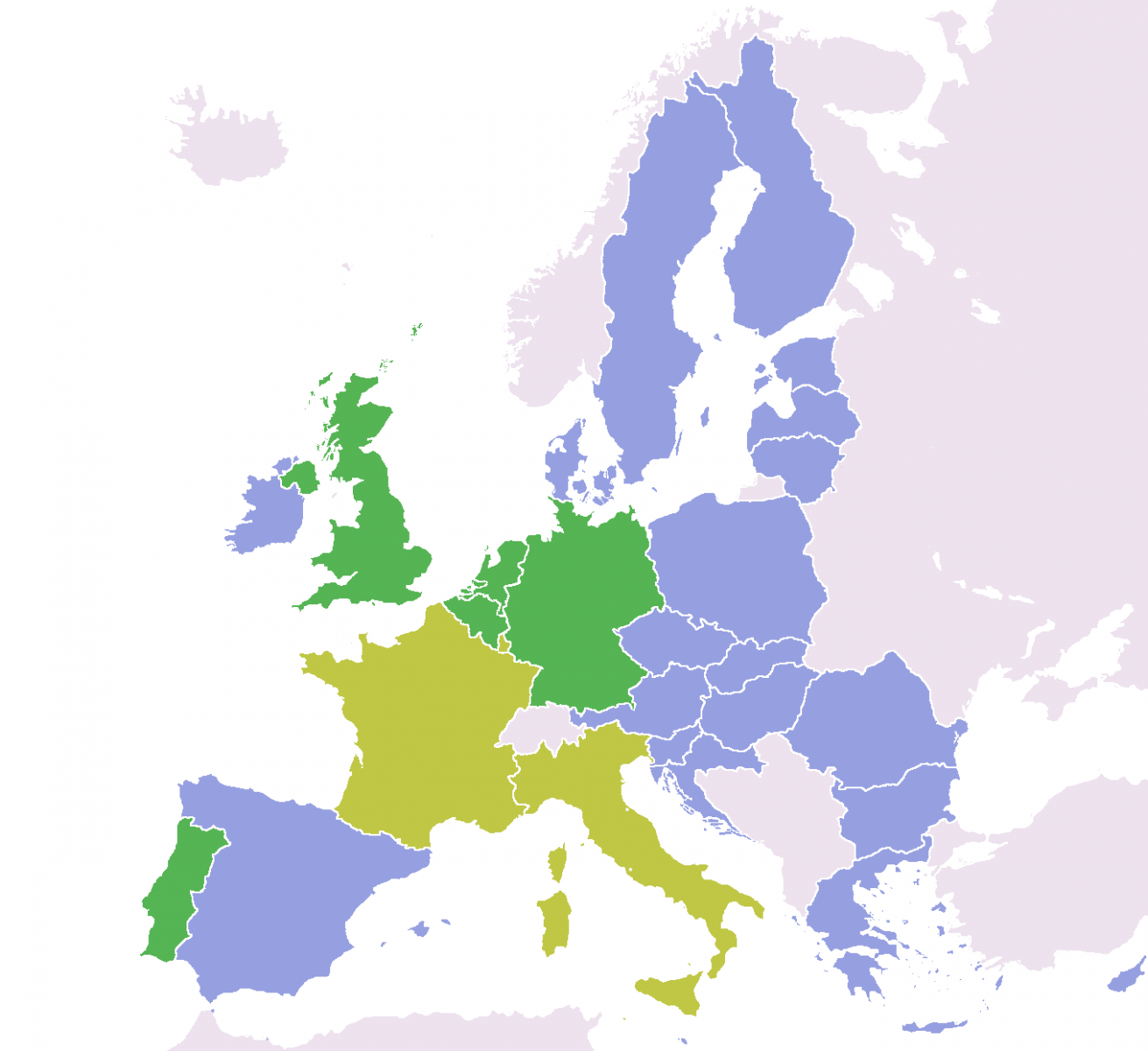
European Commission make country specific recommendations on health and hospital care
As part of its annual Country Specific Recommendations (CSR) exercise, the European Commission has singled out countries to make particular recommendation about the operation of their health systems. The countries include: Austria, Bulgaria, Czech Republic, Finland, France, Germany, Ireland, Latvia, Poland, Portugal, Romania, Slovakia and Spain.
Overall, the recommendations emphasise the need to ensure cost-effectiveness and sustainability of health systems and call for concrete, targeted reforms to optimise the hospital sector, strengthen primary care and rationalise pharmaceutical spending.
- For Austria, the Commission warns: “Efficient allocation of resources in the Austrian health system is hampered by a complex governance structure and a relatively strong focus on the large and costly hospital sector. Some measures have been taken to implement health care reform and to increase the cost-effectiveness of public spending. However, they may not be sufficient to address structural weaknesses in the sector and there remains a need to set more ambitious targets for shifting from inpatient to outpatient care and to reinforce preventive health care, for which public spending is below EU average.”
- For Bulgaria, the Commission points out that the country: “faces important challenges in the rationalization and management of the hospital sector, including a lack of transparency in hospital financing and insufficiently developed services for out-patient care. Furthermore, the high level of formal and informal payments borne directly by the patient effectively excludes certain segments of the population from access to health-care. Health status indicators are weak in comparison with other Member States, indicating that structurally higher public expenditure on health may be required in the future.”
- For the Czech Republic, the Commission advises: “Take measures to improve significantly the cost-effectiveness and governance of the healthcare sector, in particular for hospital care.”
- For Finland, the Commission recommend the country: “ensure effective implementation of the on-going administrative reforms concerning municipal structure and social and healthcare services, in order to increase the cost-effectiveness in the provision of public services”
- For France, the Commission recommends: “curbing healthcare and pension costs, for example through setting more ambitious annual healthcare expenditure targets”. “Areas where efficiency should be enhanced include pharmaceutical and administrative spending as well as hospital care.”
- In relation to Germany, the Commission believes that “only limited progress has been made…in enhancing the cost effectiveness of public spending on healthcare” and that “additional efforts are required”.
- For Ireland, there is implicit criticism of spending on health: “Even though Ireland has a relatively young population, public healthcare expenditure was among the highest in the EU in 2012 at 8.7% of GNI, significantly above the EU average of 7.3%. Given the current difficulties in managing the health budget, expected demographic pressures due to an ageing population mean that current service levels can be maintained only if value-for-money gains are achieved over the medium to long term“ Costs of medicines are also highlighted: “The high level of pharmaceutical expenditure is another challenge, with expenditure on out-patient drugs being comparatively high.” The Commission therefore recommends advancing the reform of the healthcare sector and pursuing “additional measures to reduce pharmaceutical spending, including through more frequent price realignment exercise for patented medicines, increased generic penetration and improved prescribing practices”.
- For Latvia, the Commission states: “access to healthcare is hampered by costs, including high out-of-pocket payments and prevalent informal payments, leaving a high proportion of the population with unmet health-care needs. There is significant room to enhance the efficiency of the system, ensure cost-effective financing and promote disease prevention activities.”
- For Poland, the Commission recommends: “The burden on public finances could be lowered and the access to healthcare improved through strengthening primary care and referral systems and exploiting the potential for cost-efficiency gains in hospital care”.
- For Portugal, the Commission recommends the country: “Control health care expenditure growth and proceed with the hospital reform”
- For Romania, the Commission recommends: “Inefficient use of resources and poor management increase the fiscal sustainability risk in the health sector. Widespread informal payments in the public healthcare further hinder the accessibility, efficiency and quality of the system. Reforms to improve the efficiency of the healthcare sector and its financial sustainability have begun but continuous efforts are needed. Some of the measures are incurring delays and suffer from insufficient funding and the services' low capacity. Reducing the excessive use of hospital in-patient care and strengthening primary care and referral systems will increase cost-effectiveness.”
- For Slovakia, the Commission recommends improving “the long term sustainability of public finance by increasing the cost-effectiveness of the health-care sector, in particular by rationalising hospital care and management and by strengthening primary care.”
- For Spain, the Commission recommends continuing to “increase the cost-effectiveness of the health-care sector, in particular by further rationalising pharmaceutical spending, including in hospitals and strengthening coordination across types of care, while maintaining accessibility for vulnerable groups.”
General information here.
Country specific recommendations here.
EU Funding opportunities: National information days

Information days on how to obtain funding from the European Union (EU) for health related projects will take place across EU countries in the coming weeks.
The EU is commencing its third “Health Programme” (2014-2020) this year, a 450m euro package with grants available for:
- cooperation projects at the EU level,
- actions jointly undertaken by Member State health authorities,
- the functioning of non-governmental bodies, and
- cooperation with international organisations.
To help individuals and organisations better understand the opportunities available to them via the funding programme, a series of information days are being organised at the national level. Scheduled and publicised so far are:
- Bulgaria (2nd half of June tbc)
- Croatia (2-5 July)
- Czech Republic (17 June)
- Finland (August tbc)
- Italy (12-13 June)
- Lithuania (13 June)
- Norway (Oslo on 19 June and Trondheim 27 August)
- Poland (12 June)
- Portugal (23 June)
- Slovak Republic (2nd half of June tbc)
- Slovenia (13 June)
- Spain (24 June)
- UK (11 July)
More information about the national information days here.
More information about the EU Health Programme here.
Final text of new EU Clinical Trials Regulation now published in the Official Journal of the EU

The last stage of legislative process for reforming clinical trials regulation in the EU was completed last week with the publication of the full text of the new regulation in the Official Journal of the European Union, signed on behalf of the Presidents of the European Parliament and the Council of Ministers (EU national Governments).
The Regulation now moves into an implementation phase, with the European Medicines Agency already commencing work on the construction of a single electronic portal for trial authorization submission. Implementation is hoped to be achieved by mid-2016.
See EAHP EU Monitor 15 April 2014 for more information on the content of the Regulation.
Regulation published in the Official Journal of the European Union here.

EJHP: Screening for physicochemical incompatibilities of intravenous drugs in intensive care units
A recent report in the European Journal of Hospital Pharmacy (EJHP) investigates the issue of screening for physicochemical incompatibilities of intravenous drugs in intensive care units – in particular the case of monobasic potassium phosphate and furosemide.
Physicochemical incompatibilities between intravenous drugs are a recurrent problem in intensive care units (ICUs) where most of the drugs are administered continuously. The investigation team thus conducted a literature search on the topic and performed visual assays to assess compatibilities and incompatibilities.
The full report and conclusions are available here.