 The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
You can subscribe to receive the EAHP EU Monitor by email HERE.
 EAHP members adopt 5-year plan for implementation of the European Statements of Hospital Pharmacy
EAHP members adopt 5-year plan for implementation of the European Statements of Hospital Pharmacy
The recent General Assembly of the European Association of Hospital Pharmacists (EAHP) has approved the appointment of a dedicated team to lead activity and initiatives to assist the implementation of the 44 European Statements of Hospital Pharmacy across Europe.
Main points of the implementation plan include:
- Appointment of national implementation ambassadors. They will work as a link between EAHP, member associations and the work that is done within their countries.
- Launch of an awareness campaign. Content will be presented by October 2016 and the full campaing will be launched by March 2017.
- Design of national strategies to map out and approach relevant stakeholders.
- Development of a self-assessment tool for hospital pharmacists to assess their level of implementation and develop action plans accordingly.
More information HERE.
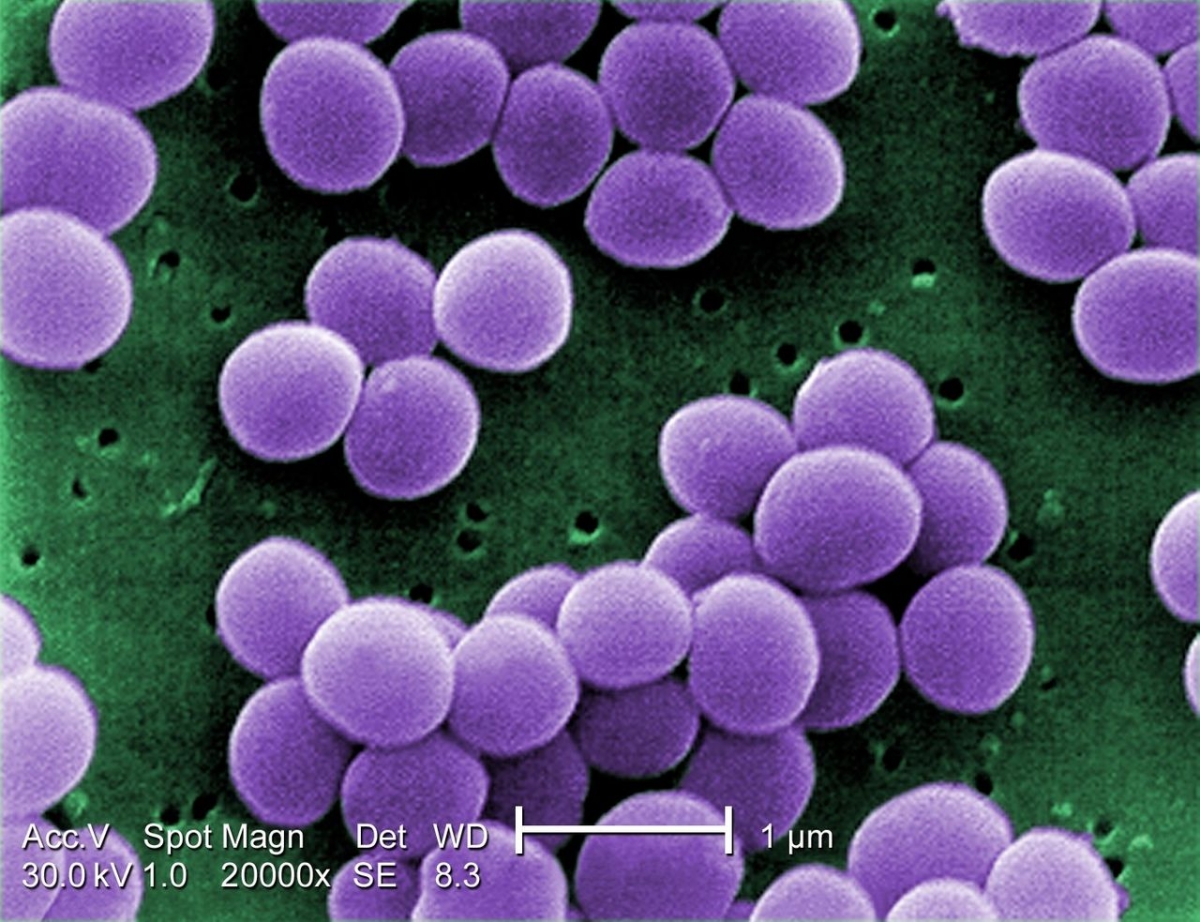
BRIEFING: Consultation on EU guidelines on the prudent use of antimicrobials in human medicine
The European Centre for Disease Prevention and Control (ECDC) has opened an important consultation on EU guidelines on the prudent use of antimicrobials in human medicine. The consultation closes on Monday 5th September.
The Guidelines are being developed following a request to the EU agency by the European Commission. They include good clinical practice and the resources, systems and processes that the various authorities and actors should consider in the development and implementation of strategies for EU health systems to support and promote the prudent use of antimicrobials.
Amongst the highlights within the current draft guidelines are strong calls for:
- All EU Governments to fund, develop and implement national action plans for appropriate use of antimicrobials in human medicine;
- The setting of qualitative and quantitative targets for improvement of prescribing;
- Ensuring availability of standardised local and national open data for benchmarking;
- Ensuring national clinical guidance is reviewed and revised when there is a significant change in antimicrobial resistance;
- The establishment of lists of antimicrobials with restrictive measures for use;
- Incentive systems for appropriate prescribing; and,
- Common antimicrobial stewardship programmes covering hospitals, primary care and long-term care facilities at national and regional level.
The appendix to the guidelines provides a list of proposed examples of quantitative indicators to be used in respect to prudent use of antimicrobials in human medicine, including:
- Number of Full Time Equivalents (FTEs) for antimicrobial stewardship activities;
- Proportion of prescriptions compliant with guidelines; and,
- Incidence of Clostridium difficile infections.
Commenting on the guidelines and the consultation, Tajda Miharija Gala, EAHP Vice-President and policy lead on antimicrobial resistance, said:
“While it is very welcome that an EU initiative is being undertaken to improve antimicrobial stewardship across Europe, a first review of the document suggests much more could be included in respect to improving stewardship in hospitals. An example includes better reflection of the O’Neill report’s recommendation that funding for antimicrobial specialists be enhanced.
The role of the hospital pharmacist in antimicrobial stewardship team, including reviewing and advising on prescription and prescription policy, conducting therapeutic drug monitoring, counseling healthcare practitioners in interactions between antimicrobials and other medication, and counseling patients in antibiotic use at discharge, among other activities, appears under-described in the guidance as well.
EAHP is now preparing a response to this effect, and we welcome all contributions of national and regional good practice for inclusion.”
Hospital pharmacists can contribute views on the guidelines, and the EAHP response, to info [@] eahp.eu.
More information HERE.
 BRIEFING: European Commission consults stakeholders on mHealth assessment guidelines
BRIEFING: European Commission consults stakeholders on mHealth assessment guidelines
The European Commission is creating EU guidelines on assessing of the reliability of mobile health applications, and is inviting interested stakeholders to respond with comments to an early draft by a deadline of 31 August 2016.
The guidelines are intended to “propose a set of common quality criteria and assessment methodologies to help different stakeholders including end users, developers, payers of care, and vendors of electronic health record systems to assess the validity and reliability of mHealth apps“.
As voluntary guidelines, they are intended to address the so-called ‘grey zone’ of apps that just fall below the lowest category of medical device regulation (Class 1), through to apps such as medical appointment booking apps that nevertheless involve exchange of potentially sensitive personal information.
‘Off-label’ uses of apps with other intended use(s), in other words, apps being used in the health or social care context for which they were not originally intended, are excluded from the scope.
Benefits intended to be delivered by the guidelines include:
- Enabling patients to give health professionals access to data collected by the apps for the purpose of improved consultations;
- Providing an assessment tool for healthcare professionals when choosing or recommending an app; and,
- Positioning of app assessment processes in the context of evidence of clinical effectiveness.
Nine criteria have been identified as relevant to the assessment of mHealth apps:
| 1. Reliable |
4. Safe |
7. Usable |
| 2. Desirable |
5. Secure |
8. Effective |
| 3. Credible |
6. Transparent |
9. Stable |
The listed criteria are then supplemented with suggested models for assessing apps against the criteria, including via assessment questionnaire. Case studies of mHealth app assessment approaches from across Europe, including the United Kingdom, the Netherlands, and Catalonia, are included for discussion.
Commenting on the consultation, EAHP Board Member Robert Moss, and member of the European Commission’s mHealth assessment guidelines working group, said:
“Through this initiative, the European Commission is responding to stakeholder concerns about the emerging mHealth landscape. This includes addressing issues such as clinical evidence, claims on the purpose and function of apps, and testing and validation. However, I believe there is still much scope to firm up the guidelines in a number of areas. Loose wording can lead to wide interpretation and one can imagine ultimately needing to revisit the guidelines in future if this is the case. EAHP’s response will therefore give a focus to this area of improvement, and have in mind apps that especially impinge on hospital practice, such as dose calculators, adherence apps, and apps that collect or process health-related data which can be integrated in electronic health records.”
More information HERE.

EJHP article explores implementation of the Falsified Medicines Directive in Poland
A new article has been published in the European Journal of Hospital Pharmacy examining the background, implementation and potential recommendations for pharmacists relating to implementation of the Falsified Medicines Directive (FMD) in the pharmacy sector, with particular attention on the case study of Poland.
The article concludes with a series of arising recommendations for hospital pharmacists, including:
- Introduction of the FMD in hospital pharmacies will be difficult and consequently, hospital managers need to be familiar with the new legislation framework;
- Implementation of the FMD is an opportunity to promote new services into routine practice and to broaden the concept of pharmaceutical care;
- Hospital pharmacists should analyse their workflow and their dispensing operations to better understand how they will implement FMD requirements in their hospital; and,
- Standard operations procedures should be adopted in hospitals to ensure good authentication practices for medicines.
Commenting on the article, EAHP Board Member Dr. András Süle, and policy co-lead on the Falsified Medicines Directive, said:
“This is a welcome article that contributes to the thinking that all hospital pharmacy leaders need to conduct about how they will deliver compliance with the Falsified Medicines Directive’s requirements for authentification scans of medicines. This will be a hot topic for hospital pharmacy in all EU and EEA countries, and I encourage all hospital pharmacists to develop their familiarity “.
More information HERE.
The Falsified Medicines Directive will form an important part of the Scientific Programme of the forthcoming EAHP Congress in Cannes, 22-24 March 2017. More information HERE.
Registration for the Congress is now open. More information HERE.
 EAHP President congratulates Irene Krämer on prestigious national award in recognition of hospital pharmacy achievements
EAHP President congratulates Irene Krämer on prestigious national award in recognition of hospital pharmacy achievements
Prof Dr Irene Krämer, Director of the Pharmacy Department at the Medical Center of Johannes Gutenberg-University Hospital in Mainz, has been awarded one of the highest civic honours in Germany, the Cross of the Order of Merit of the Federal Republic of Germany (Bundesverdienstkreuz).
The award was made in recognition of her outstanding contributions within the field of pharmacy, including in the development of clinical pharmacy services, and in the conduct of scientific research.
Professor Krämer has made enormous contributions to both EAHP’s member association in Germany, Bundesverband Deutscher Krankenhausapotheker (ADKA), as well as the educational and professional development activities of the European Association of Hospital Pharmacists (EAHP).
Commenting on the award, EAHP President Joan Peppard remarked:
“Professor Krämer represents the best in the hospital pharmacy profession. An innovator, a leader, and an educator, she’s driven by the motivation of improving care for patients. It is always a delight to see any hospital pharmacist emerge into the spotlight and gain recognition for their endeavours. On behalf of EAHP, I send Professor Krämer our warmest congratulations“.
More information HERE.
 Current consultations of hospital pharmacy relevance
Current consultations of hospital pharmacy relevance
- Four European Commission consultations on clinical trial regulation.
Deadline 31 August 2016.
More information HERE.
- European Commission consultation on mHealth assessment guidelines.
Deadline 31 August 2016.
More information HERE.
- ECDC consultation on EU guidelines on the prudent use of antimicrobials in human medicine.
Deadline 5 September 2016.
More information HERE.
























 The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe.
The EAHP EU Monitor is a regular round up of news relevant to hospital pharmacy in Europe. EAHP members adopt 5-year plan for implementation of the European Statements of Hospital Pharmacy
EAHP members adopt 5-year plan for implementation of the European Statements of Hospital Pharmacy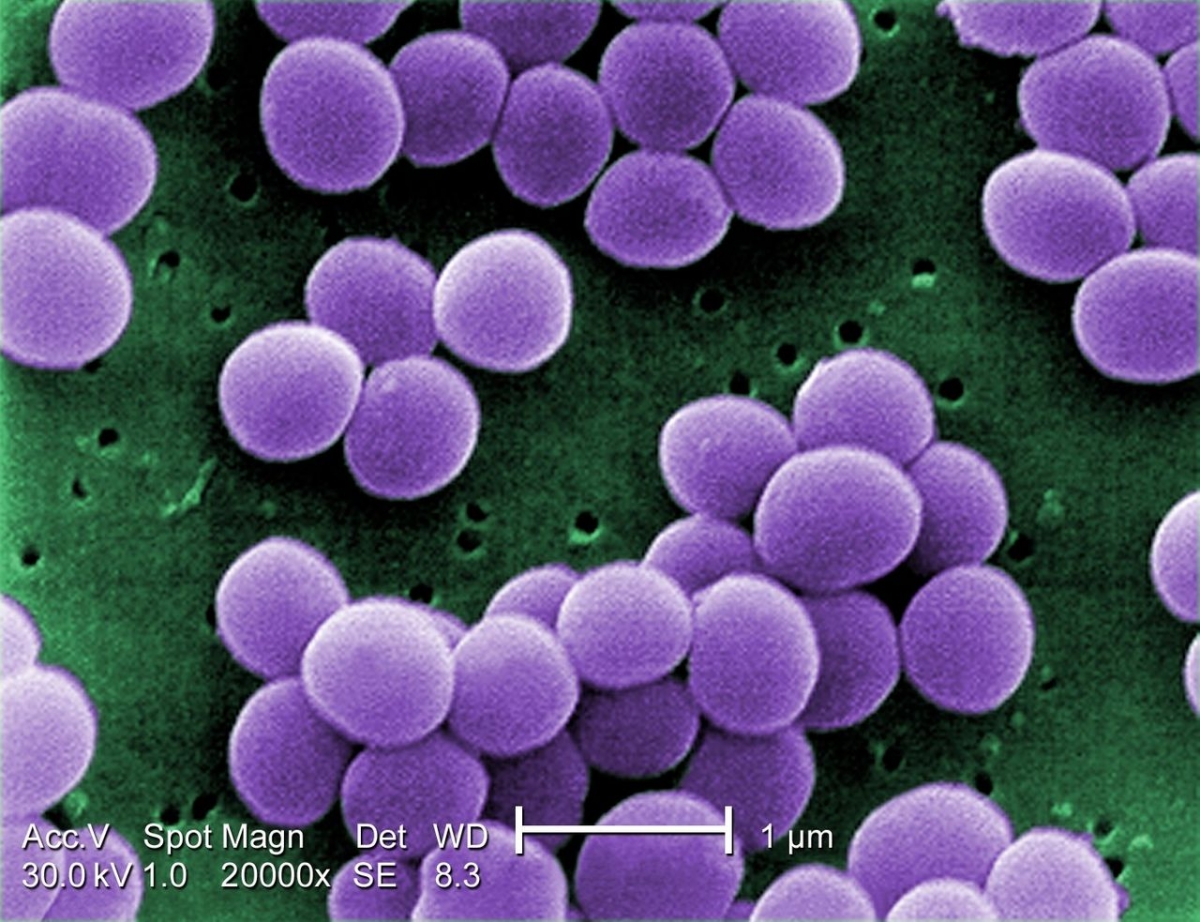
 BRIEFING: European Commission consults stakeholders on mHealth assessment guidelines
BRIEFING: European Commission consults stakeholders on mHealth assessment guidelines
 EAHP President congratulates Irene Krämer on prestigious national award in recognition of hospital pharmacy achievements
EAHP President congratulates Irene Krämer on prestigious national award in recognition of hospital pharmacy achievements Current consultations of hospital pharmacy relevance
Current consultations of hospital pharmacy relevance